Immediately after Donald Trump won the election, women across the U.S. started looking into safe birth control options that could outlast his administration—myself included.
Earlier this year, Planned Parenthood reported a 900 percent increase in women seeking out IUDs (intrauterine devices), many of which have a lifespan of at least a one-term presidency. Then in 2017, the Trump administration rolled back the federal mandate that requires employers to cover birth control and introduced the tax bill that disproportionately affects low-income women. As 2018 approaches, even more women are driven toward long-term solutions for reproductive healthcare.
Despite the looming threat of decreased accessibility, we’re at least not short on birth control options: birth control pills, birth control patches, rings, implants, shots, and of course condoms, along with other emergency contraceptives. But when weighing the pros and cons, the birth control option that often comes out on top is the IUD.
I’ll proudly call myself an IUD evangelist, regularly gabbing to friends and strangers about my experience. It’s long-term, reversible, effective, and simple. But politics aside, getting an IUD was a carefully considered personal choice that took a lot of research and preparation. If you’re considering joining the club, here’s what you need to know about how an IUD works, and if it will work for you.
In the spirit of things morally objectionable, let 👏me 👏tell 👏y’all 👏about 👏my 👏IUD
— Lauren L’Amie (@laurenlamie) October 6, 2017
What is an IUD?
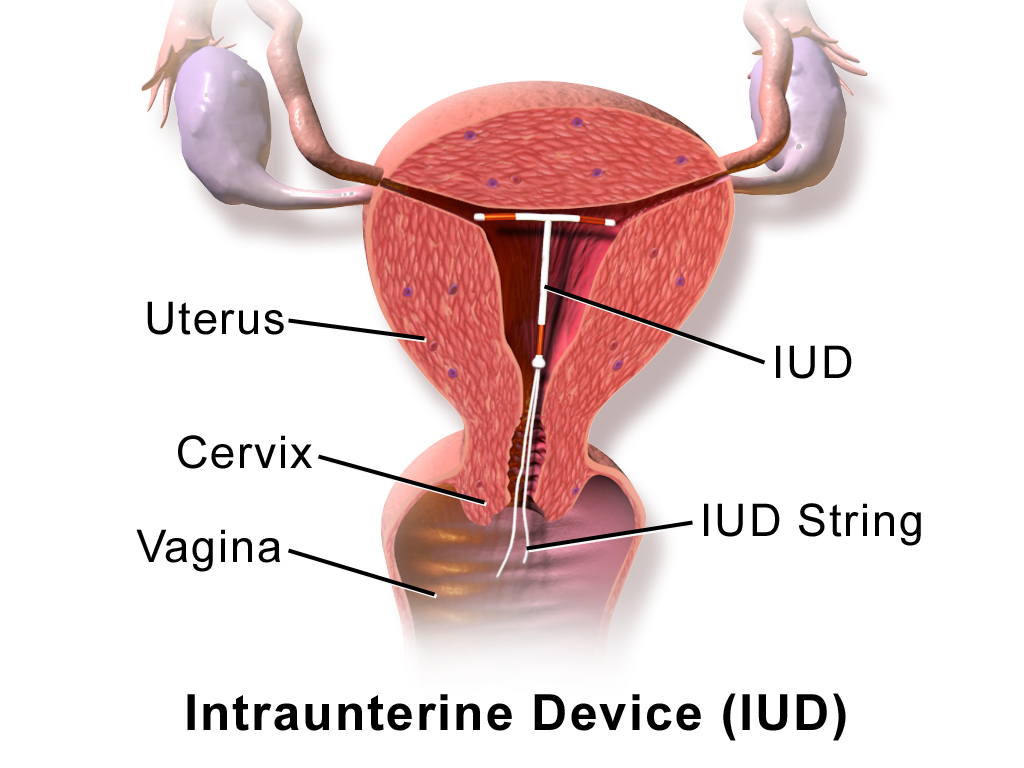
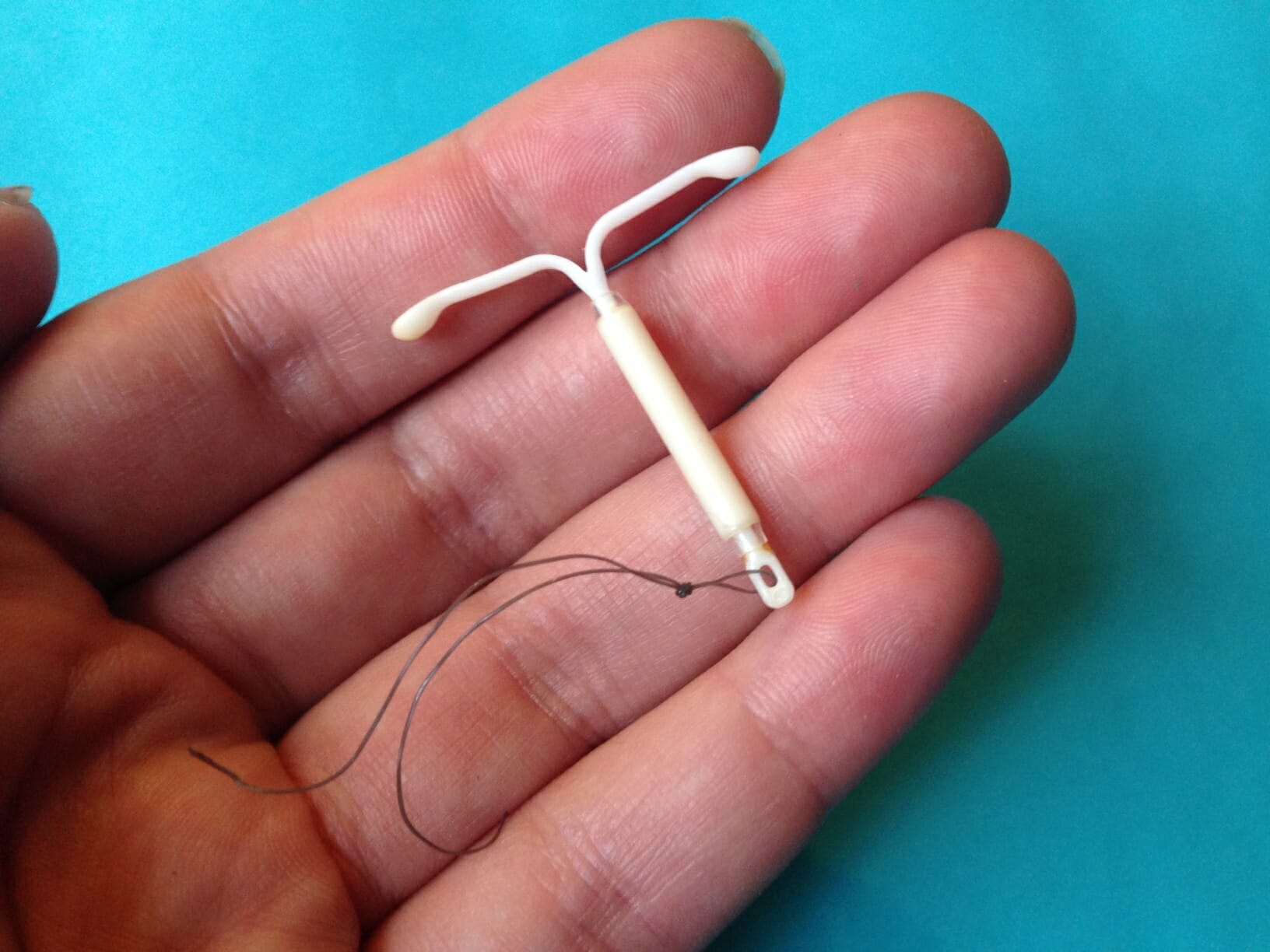
An IUD, or intrauterine device, is a small T-shaped device that is inserted into the uterus by a physician to prevent pregnancy for up to 12 years. Along with hormonal implants, IUDs are pretty much the best of the best when it comes to long-term birth control—they’re more than 99 percent effective compared to the birth control pill, which can be up to 99 percent effective. Those extra percentage points, along with long-term pregnancy prevention, are what draw many women to choose the IUD.
How do IUDs work?
IUDs primarily work to prevent fertilization. An IUD sits in the uterus with both arms of the “T” stretching out to touch both sides. The core of the IUD reaches down to the cervix, where removal strings reach down into your vagina.
There are two types of IUDs: copper and hormonal. Nonhormonal copper IUDs are wrapped in a thin, pure copper wire that acts as a spermicide within the uterus. Hormonal IUDs contain progestin (the same hormones in the birth control pill) that stops the process of ovulation in your ovaries. They also thicken the cervical mucus to block sperm from entering the uterus.
READ MORE:
- The financial costs of an uninsured abortion
- How does federal funding for Planned Parenthood actually work?
- 11 important things you didn’t know about Planned Parenthood
- When was birth control invented? A brief history of the pill
Which brand should I choose?
Choosing which IUD is right for you means considering what you prefer when it comes to pregnancy prevention. If you opt for a non-hormonal option, the copper IUD—ParaGard—is currently the only brand available. ParaGard can remain in place for 10 to 12 years, making it the longest-lasting IUD available, but it has also been linked with worse menstrual cramps and heavier periods.
Hormonal IUDs (like Mirena, Skyla, Kyleena, Liletta) are typically recommended for women who haven’t had children or who have only had one child. They also last for shorter periods of time. Mirena lasts up to six years, Kyleena lasts up to five years, Liletta lasts up to four years, and Skyla lasts up to three years. All hormonal and nonhormonal options can be removed at any time by your physician.
I have Kyleena, which I chose because I switched from the hormonal birth control pill and it never left me with any unwanted side effects. If anything, the hormones have cleared my skin and helped to regulate my period. She’s been nothing but a welcome friend so far, and we have four more presumably blissful years together.
Does getting an IUD hurt?
I’m not going to tell you it doesn’t. You may have heard horror stories about insertion, but the amount of pain during and after insertion is variable. Every woman has a different experience. For me, it felt like an excruciating pinch that lasted for one minute, followed by a couple days of cramps, irregular bleeding, and discomfort. But like many other women, I see that momentary pain as a fair trade for reliable birth control, peace of mind, and overall better sex, periods, and hormone regulation.
In order for an IUD to be inserted into your uterus, it has to go through your cervix. In case you didn’t already know, that’s the same narrow opening between the uterus and vagina that dilates during childbirth. Depending on the relative size of your cervix and the IUD you choose, your physician may prescribe cervix-softening drugs before your insertion.

In any case, take several painkillers (like Advil or Motrin) prior to your insertion. Stay hydrated and eat a good meal before the procedure, especially if you are prone to fainting. It’s also a good idea to prepare to be in recovery for at least a couple days afterward, even if you feel fine. Take a sick day if you can or make sure you have someone on hand to care for you (or at least bring you a heating pad and make you tea).
What are the side effects after insertion?
According to Planned Parenthood, you should expect cramps in your uterus and back immediately after insertion and spotting or irregular periods for 3 to 6 months.
Serious side effects are rare, but it’s important to know the risks involved with getting an IUD. You shouldn’t get an IUD if you’ve had cervical cancer or cancer of the uterus, or if you might already be pregnant. In very rare cases, the IUD can slip out of the uterus or tear the uterine wall. If this happens, you’ll definitely know and will likely have some pretty awful cramps. It’s also possible (but extremely unlikely) to get pregnant while you have an IUD. If this happens, your chances of an ectopic pregnancy are much higher.

Why do I have to be on my period when it’s inserted?
Your doctor will schedule your IUD insertion to take place while you’re on your period. This sounds messy, sure, but it’s done to ensure that you aren’t pregnant at the time of insertion. If you’re already using a method of birth control like the pill, you’ll schedule your insertion for your next period.
READ MORE:
- The woman-led quest for the best condom on the market
- Double your pleasure with these sex toys for couples
- Do condoms expire? Here’s how long they really last
- Here’s the real truth about getting pregnant on your period
What’s the deal with IUD strings?
Most physicians recommend that you regularly check the strings yourself, which is easy to do on your own by feeling inside your vagina. Yes, your partner may be able to feel the strings during sex, but probably not for long. As time goes on, the strings soften and will curl up around your cervix.
This isn’t necessarily a bad thing, but if you’re concerned and can’t feel the strings at all (or if they’re irritating you every day or during sex) contact your doctor and ask to adjust or trim them.
When was the IUD invented?
Before you unceremoniously plop something into your uterus for three to 10 years, it’s totally reasonable to ask exactly where it originated from. At least, that’s what I wanted to know. The IUD might seem like a new method of contraception, but it’s actually been around since the early 1900s. The very first IUD was developed in Germany, wasn’t widely used, and was made of silkworm gut. Don’t worry, since then, the device has evolved quite a bit. The late ’50s and early ’60s brought the advent of plastic IUDs and the signature “T” shape.
The hormonal IUD was invented in the ’70s. Mirena, the first hormonal brand, was the target of several lawsuits after it caused several uterus tears and other painful side effects for users. Again, if you’ve heard of horror stories like this, know that they’re very rare today. Ask your doctor about any specific concerns with the brand you choose.
How much does an IUD cost?
IUDs can cost anywhere from $0 to more than $1,000, which is a huge range. But it depends on your health insurance plan or access to Medicaid or other government programs, which can make the IUD free or low-cost.
Keep in mind that the cost covers the device, insertion procedure, and follow-up appointments. For instance, my device was covered but I owed a co-pay of nearly $400. I was able to pay in installments, but this isn’t always the case. Check with your insurance provider, call your local Planned Parenthood, and read up on other resources before you schedule your insertion.
Still looking for clarity? Here’s what you should know about the morning after pill, all the best birth control options, the ultimate guide to getting consent, and how federal funding works for Planned Parenthood. Plus, read up on the history of birth control.
Editor’s note: This article is regularly updated for relevance.


